Bacterial Balance
The bacterial balance in the intestine and how this may predispose to autoimmune disorders. The effects of different diets on bacteria in the intestine.
How do the multi-trillion population of bacteria in your intestine affect your immune system?
Wow…an estimated 75% of the immune cells in the human body are found in the GI tract. (1) This is a major influence on how the rest of your immune system reacts. The immune cells in your lungs know…any microbe is the enemy. But in the gut, the immune system must decide, is this a friend or a foe? The intestinal microbiota has a critical role in development of immunity. It can also protect from pathogens (disease causing bacteria, molds or viruses) directly by preventing their attachment, as well as outcompeting them for nutrients, and maintaining pH.
During vaginal delivery, the infant is exposed to its first dose of probiotics as it swallows the fluids in the birth canal. Cesarean Delivery increases chances of developing celiac disease with a 1.8 odds ratio (2)
A correlation has been found between intestinal bacterial balance and development of autoimmune diseases. Examples of associations between intestinal bacteria and autoimmune disease:
- Klebsiella: Ankylosing Spondylitis
- Citrobacter, Klebsiella, Proteus Rheumatoid Arthritis
- Yersinia: Grave’s Disease & Hashimoto’s Disease
- S. Pyogenes: Rheumatic Fever
- Helicobacter pylori: Hashimoto's
- Camphylobacter jejuni: Gullian Barre Syndrome (3)
Some studies have found that celiac patients have different bacteria in their stool from the general population. This may correlate with the fact that celiac patients have approximately 10 times the rate of auto-immune thyroid diseases, such as Hashimoto’s thyroiditis and Grave’s disease, as non-celiac individuals (4)
Bacteria may play a role in other diseases, as well. Clostridium coccoides produce short chain fatty acids. Some short chain fatty acids, such as propionic acid, are helpful in low quantities, but neurotoxic in high quantities and may contribute to the development of Autism symptoms (6,7). Diet and its effects on the Microbiota have been linked with depression (8,9)
If an imbalance in the microbiota is harmful, how can I impact the balance the most? Most people would say to take a probiotic. But, if you aren’t feeding a probiotic the right food, it may not help. I would say a probiotic is important, but so is diet. ~60% of gut microbiota variability can be attributed to food.
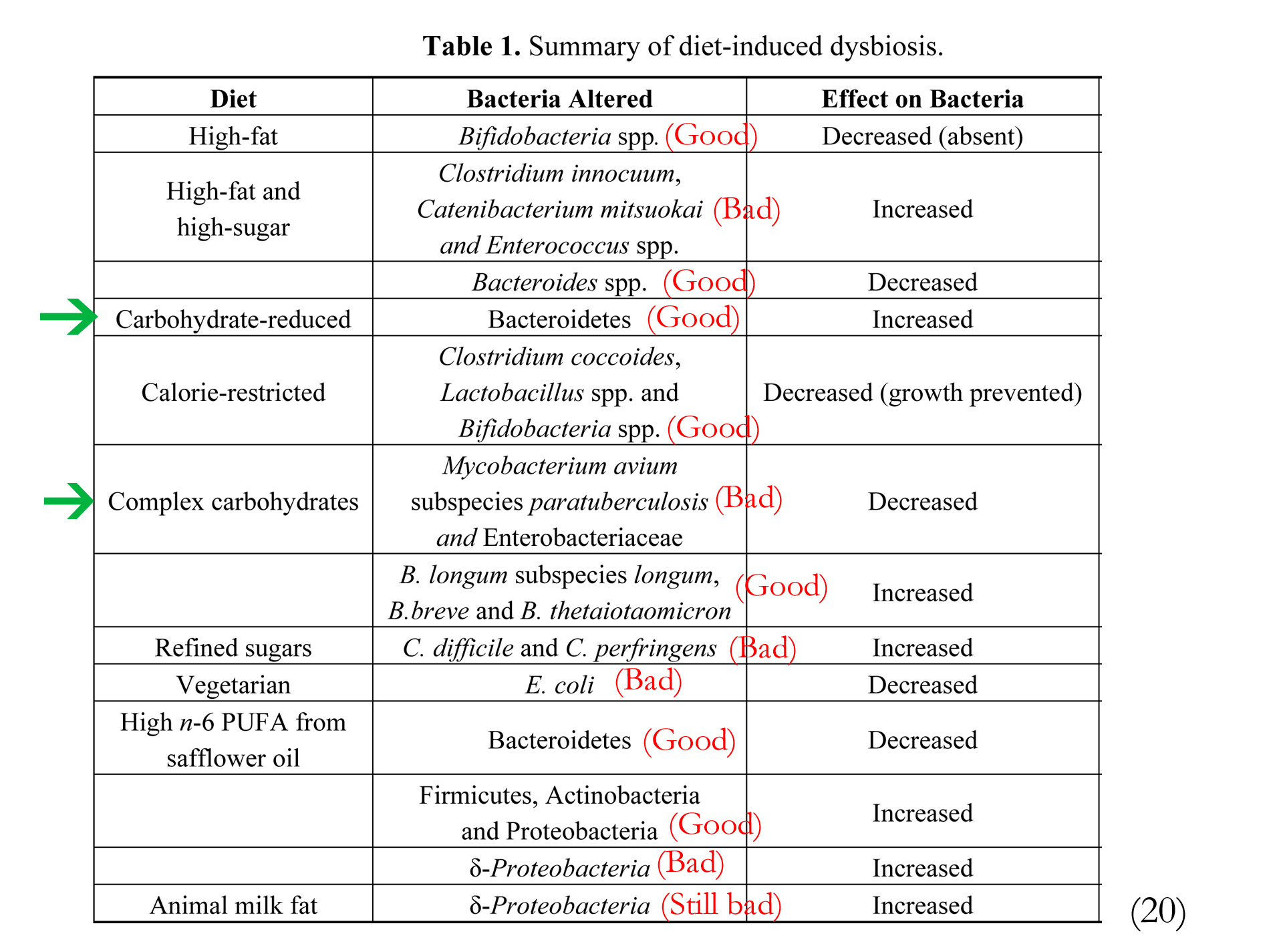
How does diet affect the intestine? Lets look at the first food humans receive. Breast fed infants have higher levels of Bifidobacteria spp. while formula fed infants have higher levels of Bacteroides spp., as well as increased Clostridium coccoides and Lactobacillus spp. (5) The following chart shows the affect of different diets on Bacteria.
A gluten-free diet decreases the number of Firmicutes and increases the quantity of Proteobacteria. In celiac individuals this may cause a reduced immune response. A gluten-free diet may not completely restore the microbial balance. Administration of Lactobacillus casei has been found to be effective in restoring the mucous layer and lymph integrity in a mouse model of celiac (10-13).
Probiotics in small doses (1-2 million) are not enough to even make a drop in the bucket. There are 10 trillion cells in your body and about 100 trillion microbes in your intestines. It takes consistent dosing of acid-resistant strains. I recommend 20-40 billion bacteria per dose at least.
Eat 5-6 servings of non-starchy vegetables to feed the good bacteria.
References
1. Bengmark, S Acut and “chronic” phase reaction–a mother of disease. ClinNutr, Vol 23 No. 6. 1256-1266. Dec. 2004
2. Decker et al. C-Section Delivery and Increased Risk of Celiac Disease Pediatrics 2010;125:1433-40.
3. Mayes MD. Epidemiologic studies of environmental agents and systemic autoimmune diseases. Environ health perspect. 1999; 107 (suppl 5): 743-748
4. Ansaldi N et al, Autoimmune thyroid disease and celiac disease in children (Abstract), J Pediatr Gastroenterol Nutr, Vol. 37, No. 1, pp. 63-66
5. Fallani, M.; Young, D.; Scott, J.; Norin, E.; Amarri, S.; Adam, R.; Aguilera, M.; Khanna, S.; Gil, A.; Edwards, C.A.; et al. Intestinal microbiota of 6-week-old infants across europe: Geographic influence beyond delivery mode, breast-feeding, and antibiotics. J. Pediatr. Gastroenterol. Nutr. 2010, 51, 77–84.
6. El-Ansary, A.K.; Ben Bacha, A.; Kotb, M. Etiology of autistic features: The persisting neurotoxic effects of propionic acid. J. Neuroinflamm. 2012, 9, 74.
7. Donohoe, D.R.; Garge, N.; Zhang, X.; Sun, W.; O’Connell, T.M.; Bunger, M.K.; Bultman, S.J. The microbiome and butyrate regulate energy metabolism and autophagy in the mammalian colon. Cell Metab. 2011, 13, 517–526.
8. Gibson PR, Newnham E, Barrett JS, Shepherd SJ, Muir JG. Review article: fructose malabsorption and the bigger picture. Aliment Pharmacol Ther 2007;25(4):349–363. 2000;35:1048–1052.
9. Ledochowski M, Widner B, Murr C, Sperner-Unterweger B, Fuchs D. Fructose malabsorption is associated with decreased plasma tryptophan. Scand J Gastroenterol 2001;36(4):367–371.
10. Nistal, E.; Caminero, A.; Vivas, S.; Ruiz de Morales, J.M.; Saenz de Miera, L.E.; Rodriguez-Aparicio, L.B.; Casqueiro, J. Differences in faecal bacteria populations and faecal bacteria metabolism in healthy adults and celiac disease patients. Biochimie 2012, 94, 1724–1729.
11. Di Cagno, R.; de Angelis, M.; de Pasquale, I.; Ndagijimana, M.; Vernocchi, P.; Ricciuti, P.; Gagliardi, F.; Laghi, L.; Crecchio, C.; Guerzoni, M.E.; et al. Duodenal and faecal microbiota of celiac children: Molecular, phenotype and metabolome characterization. BMC Microbiol. 2011, 11, doi:10.1186/1471-2180-11-219.
12. Sanz, Y.; de Pama, G.; Laparra, M. Unraveling the ties between celiac disease and intestinal microbiota. Int. Rev. Immunol. 2011, 30, 207–218.
13. De Palma, G.; Nadal, I.; Collado, M.C.; Sanz, Y. Effects of a gluten-free diet on gut microbiota and immune function in healthy adult human subjects. Br. J. Nutr. 2009, 102, 1154–1160.
20. Brown, K et al. Diet-Induced Dysbiosis of the Intestinal Microbiota and the Effects on Immunity and Disease Nutrients 2012, 4, 1095-1119; doi:10.3390/nu4081095