Digestion & GI Health
The health of your intestine impacts the health of your whole body. One thing that can occur in the intestine that can be a major impact is “leaky gut”, or intestinal hyperpermeability. “Leaky gut”, or intestinal hyperpermeability is one of the problems that can be caused by an imbalance of bacteria in the intestine. It can also be caused by food sensitivities, chemical exposure,and inflammation. “Leaky gut” may be responsible for many symptoms throughout the body. It has been implicated as a contributing factor in eczema, itching, irritable bowel, chronic fatigue, chronic liver and pancreas disease, headache, hyperactivity, rheumatoid arthritis, diabetes, and more.
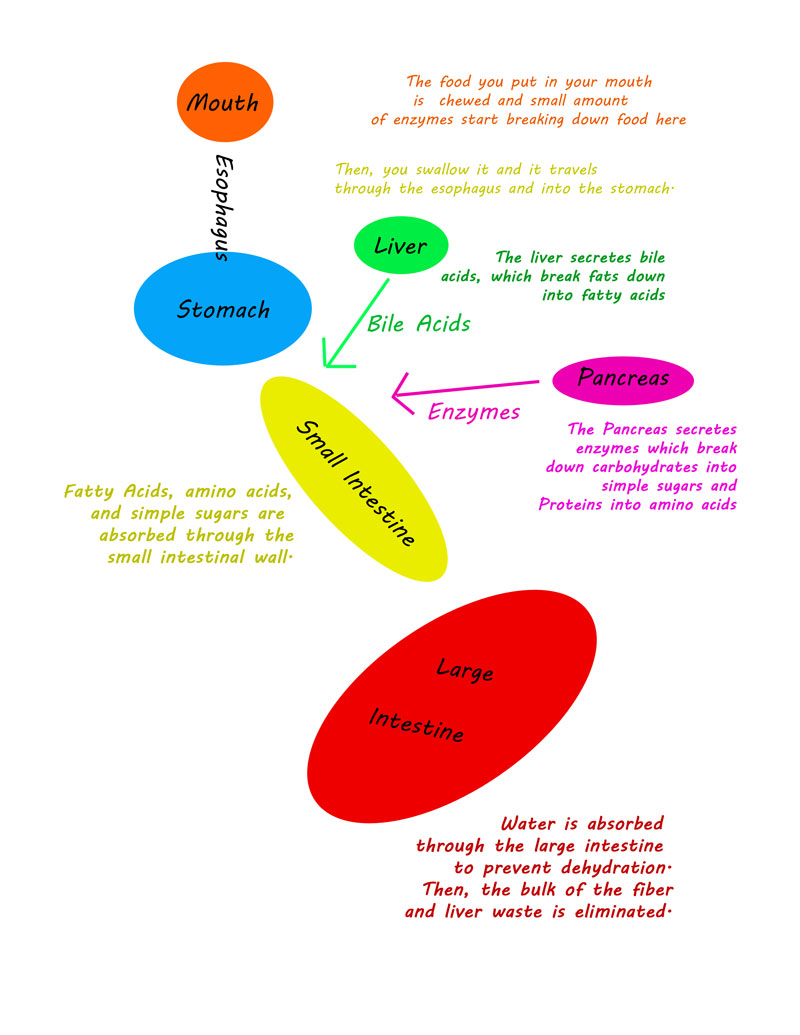
“Leaky gut” is not what it sounds like, and to dispel confusion, I will call it intestinal hypermeability. To understand intestinal hyperpermeability, one must understand the function of the intestinal cells. Let us start with a look at how your intestines are working inside of you. The following simple depiction outlines some major parts of the digestive system and what their functions are.
Since intestinal hyperpermeability occurs in the intestine, to understand what is going on, we will show a cross section of the intestine.
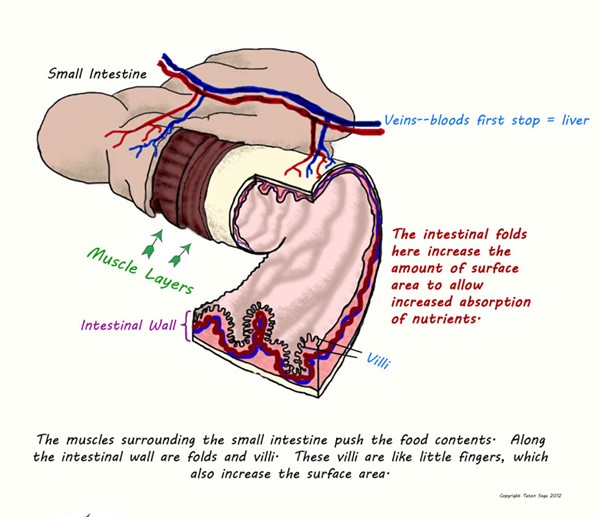
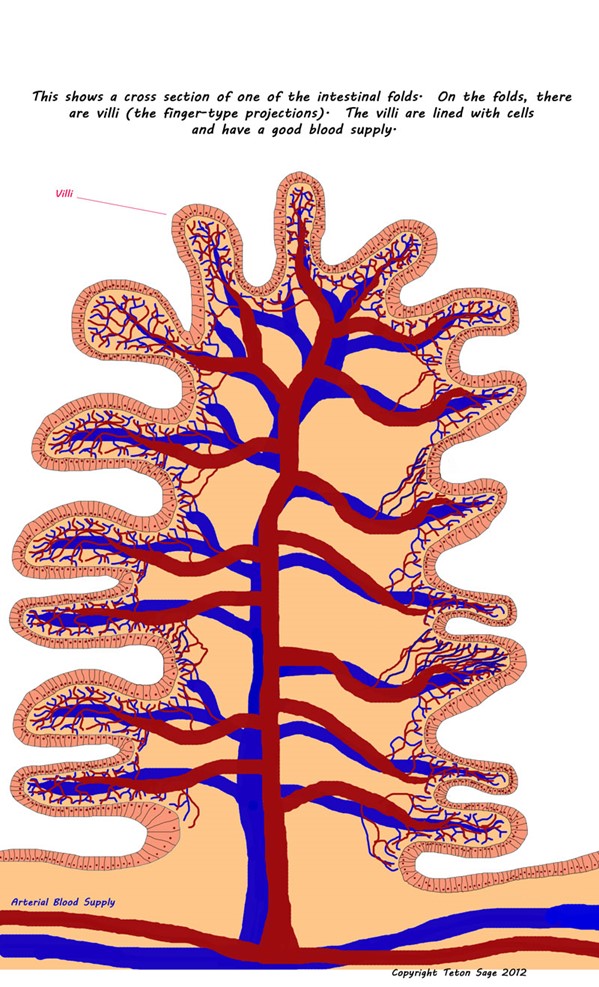
It is important to note how well the intestinal cells have a large blood supply right there. This is to help in the function of the intestine.
Normally, only fats, proteins, and carbohydrates that have been digested are allowed through the barrier lining the intestine. In the intestine, there is a barrier that protects the body from bacteria, undigested food, and foreign or harmful substances that have been ingested. This barrier is made up of a mucus layer that allows certain substances in, but doesn’t allow the normal microbes (bacteria, etc) to touch the cells lining the intestines. In this mucus are millions of antibodies (mostly Secretory IgA) and white blood cells that help protect the body. (1) In the following illustration, the picture on the top left shows a normal intestinal cell layer with a robust mucus layer and antibodies. On the bottom left is an illustration of how broken down food particles are transported across the intestinal cell layer. All substances which pass through the intestinal barrier are transported in the bloodstream to the liver, where they are metabolized or detoxified.
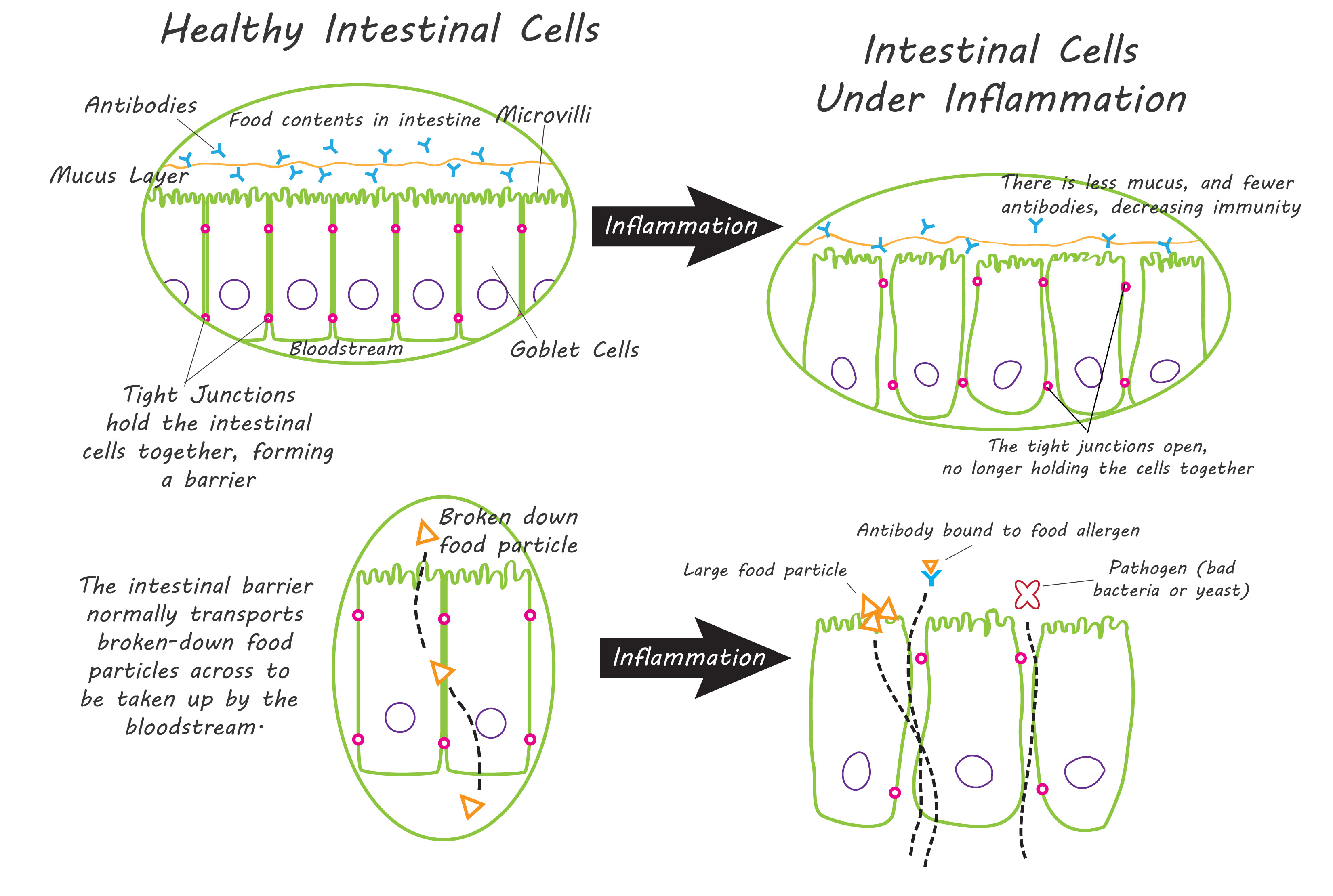
When there is inflammation or irritation to the cells, the tight junctions may not work properly if damaged. They allow larger particles to pass through into the bloodstream and straight to the liver. These larger particles may be microbes (bacteria, fungus, or virus), or un-digested food. The immune system may recognize these substances as foreign and stimulate an immune response, which causes further inflammation in the area.
These substances are then transported to the liver. There, they must be metabolized or “eaten” by the immune system. (2,3) This depletes metabolism substrates needed by the liver.
It has been shown that women with increased intestinal permeability have an increase in visceral fat (fat around the organs in the abdomen). (84) Altered intestinal permeability has also been linked with some autoimmune disorders such as Type I Diabetes (86).
The following things can contribute to an altered permeability and an increase in inflammation of the intestinal wall:
- High gluten diet
- Antibiotic use
- Proton-pump inhibitor use
- Prilosec-omeprazole
- Prevacid-lansoprazole
- Aciphex-rabeprazole
- Others
- Stress
- High alcohol intake
- Frequent NSAID use
- Advil/Motrin-ibuprofen
- Aleve/Naprosyn-naproxen
- Mobic-meloxicam
- Celebrex-celecoxib
- Others
- Helicobacter Pylori infection
- Infection of other microbiota
- Clostridium dificile
- Giardiia
- Chronic Candidiasis
- Entamoeba Histolytica
- Salmonella
- Ascaris lumbricoides
If I think this is a problem, how do I get help?
Contact me and we can discuss your symptoms and history to see what is the best option for you.